(1) Emergency readmissions to hospital within 30 days of discharge (I02040) Also broken down by: (a) age bands: <16 years, 16+ years, 16-74 years; 75+ years (b) sex: male only, female only and persons. We aimed to look at the national trends in 30-day readmission rates after CHF hospitalization. Findings This cohort study of 8 273 270 HF hospital admissions from January 2010 to December The Hospital Readmissions Reduction Program (HRRP), implemented by the Centers for Medicare & Medicaid Services (CMS), imposes a financial penalty on hospitals with higher than average readmission rates for certain conditions. Data on hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare 201319.  Unweighted, this database contains data from approximately 15 million discharges each year. 2. Hospital Utilization (in non-Federal short-stay hospitals) Data are for the U.S. Web30-Day Readmission Rates to U.S. We aimed to look at the national trends in 30-day readmission rates after CHF hospitalization. Published: July 20, 2021. 3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. WebResults National Averages Readmission Rate (1864 Years)* Readmission Rate (65 Years and Older)* Not available due to CMS suspension of data reporting during COVID-19 pandemic. Webnational award-winning (benchmark) hospitals and the median performance of non-winning (peer) hospitals in your comparison group. WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties. CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. Learn more Healthcare Insights are developed with healthcare commercial intelligence from the Definitive Healthcare platform. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. A total of 2,545 hospitals will receive lower Medicare payments for one full year due to their poor Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. *Indicates a change in ranked measures for the 2021 study edition. Readmission rates were higher during the post-HRRP penalty period compared with pre-HRRP penalty phase (all-cause readmission 30 days: 18.6% versus 17.5%, P <0.001, all-cause readmission 90 days: 32.0% versus 29.9%, P <0.001) across all subgroups except among the low-volume hospitals. Cheat sheet: Hospital readmissions reduction A recent CMS analysis of its Hospital Readmissions Reduction Program (HRRP) found that 2,500 hospitals will face HRRP penalty reductions and around 18% of hospitals will face penalties of at least 1% of their Medicare reimbursements for fiscal year (FY) 2022, Modern Healthcare reports.. Daily readmission rates decreased across most This State of Healthcare Quality Report classifies health plans differently than NCQAs Quality Compass. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. The rates per 1000 US adults for postdischarge HF readmissions (1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (0.8 in 2010 to 0.7 in 2014 to 0.9 Hospital Utilization (in non-Federal short-stay hospitals) Data are for the U.S. 1-800-557-6059 | TTY 711, 24/7.
Unweighted, this database contains data from approximately 15 million discharges each year. 2. Hospital Utilization (in non-Federal short-stay hospitals) Data are for the U.S. Web30-Day Readmission Rates to U.S. We aimed to look at the national trends in 30-day readmission rates after CHF hospitalization. Published: July 20, 2021. 3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. WebResults National Averages Readmission Rate (1864 Years)* Readmission Rate (65 Years and Older)* Not available due to CMS suspension of data reporting during COVID-19 pandemic. Webnational award-winning (benchmark) hospitals and the median performance of non-winning (peer) hospitals in your comparison group. WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties. CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. Learn more Healthcare Insights are developed with healthcare commercial intelligence from the Definitive Healthcare platform. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. A total of 2,545 hospitals will receive lower Medicare payments for one full year due to their poor Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. *Indicates a change in ranked measures for the 2021 study edition. Readmission rates were higher during the post-HRRP penalty period compared with pre-HRRP penalty phase (all-cause readmission 30 days: 18.6% versus 17.5%, P <0.001, all-cause readmission 90 days: 32.0% versus 29.9%, P <0.001) across all subgroups except among the low-volume hospitals. Cheat sheet: Hospital readmissions reduction A recent CMS analysis of its Hospital Readmissions Reduction Program (HRRP) found that 2,500 hospitals will face HRRP penalty reductions and around 18% of hospitals will face penalties of at least 1% of their Medicare reimbursements for fiscal year (FY) 2022, Modern Healthcare reports.. Daily readmission rates decreased across most This State of Healthcare Quality Report classifies health plans differently than NCQAs Quality Compass. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. The rates per 1000 US adults for postdischarge HF readmissions (1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (0.8 in 2010 to 0.7 in 2014 to 0.9 Hospital Utilization (in non-Federal short-stay hospitals) Data are for the U.S. 1-800-557-6059 | TTY 711, 24/7. 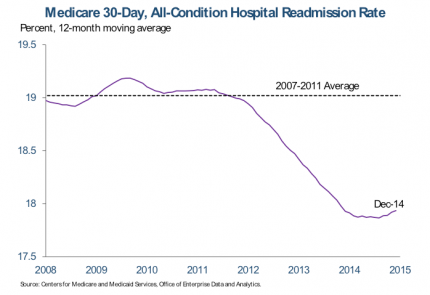 The average readmission cost was $15,200, ranging from $10,900 for self-pay/no charge stays to $16,400 for privately insured stays. Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. WebThe American Hospital Association conducts an annual survey of hospitals in the United States. In fiscal year 2021, 83 percent of hospitals evaluated were penalized . The NRD is a unique and powerful database designed to support various types of analyses of national readmission rates for all patients, regardless of the expected payer for the hospital stay.
The average readmission cost was $15,200, ranging from $10,900 for self-pay/no charge stays to $16,400 for privately insured stays. Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. WebThe American Hospital Association conducts an annual survey of hospitals in the United States. In fiscal year 2021, 83 percent of hospitals evaluated were penalized . The NRD is a unique and powerful database designed to support various types of analyses of national readmission rates for all patients, regardless of the expected payer for the hospital stay.  Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. With each patient discharge, there is a risk for 30-day readmission. Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. Hospitals by Procedure, 2010.
Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. With each patient discharge, there is a risk for 30-day readmission. Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. Hospitals by Procedure, 2010. 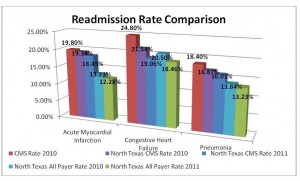 2021 Aug 1;6(8):952-956. doi: 10.1001/jamacardio.2020.7472. (1) Emergency readmissions to hospital within 30 days of discharge (I02040) Also broken down by: (a) age bands: <16 years, 16+ years, 16-74 years; 75+ years (b) sex: male only, female only and persons. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. In 2018, there were 3.8 million 30-day all-cause adult hospital readmissions, with a 14 percent readmission rate and an average readmission cost of $15,200. WebHospital-Wide The Centers for Medicare & Medicaid Services (CMS) 30-day risk-standardized readmission measures assess a broad set of healthcare activities that affect patients well-being. Hospitals by Diagnosis, 2010 and HCUP Statistical Brief #154: Readmissions to U.S. Hospital readmissions are a leading healthcare concern, both in terms of implications for the quality of care provided to hospitalized patients and for the healthcare costs associated with readmission. 2. WebResults National Averages Readmission Rate (1864 Years)* Readmission Rate (65 Years and Older)* Not available due to CMS suspension of data reporting during COVID-19 pandemic. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. The time period examined was from July 2008 to June 2016.
2021 Aug 1;6(8):952-956. doi: 10.1001/jamacardio.2020.7472. (1) Emergency readmissions to hospital within 30 days of discharge (I02040) Also broken down by: (a) age bands: <16 years, 16+ years, 16-74 years; 75+ years (b) sex: male only, female only and persons. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. In 2018, there were 3.8 million 30-day all-cause adult hospital readmissions, with a 14 percent readmission rate and an average readmission cost of $15,200. WebHospital-Wide The Centers for Medicare & Medicaid Services (CMS) 30-day risk-standardized readmission measures assess a broad set of healthcare activities that affect patients well-being. Hospitals by Diagnosis, 2010 and HCUP Statistical Brief #154: Readmissions to U.S. Hospital readmissions are a leading healthcare concern, both in terms of implications for the quality of care provided to hospitalized patients and for the healthcare costs associated with readmission. 2. WebResults National Averages Readmission Rate (1864 Years)* Readmission Rate (65 Years and Older)* Not available due to CMS suspension of data reporting during COVID-19 pandemic. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. The time period examined was from July 2008 to June 2016.  WebExplore the HCUP Fast Stats Data Tools. 2. Here are five takeaways from the Nov. 2 Kaiser Health News analysis: 1. We might expect that hospitals with more total discharges to report higher readmission rates. Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, For CMS & MIDS Contractors Only. WebKey Points. WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. 1-800-557-6059 | TTY 711, 24/7.
WebExplore the HCUP Fast Stats Data Tools. 2. Here are five takeaways from the Nov. 2 Kaiser Health News analysis: 1. We might expect that hospitals with more total discharges to report higher readmission rates. Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, For CMS & MIDS Contractors Only. WebKey Points. WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. 1-800-557-6059 | TTY 711, 24/7.  The cost of hospital readmissions is enormous, estimated to be in the vicinity of $26 billion annually (Wilson, 2019), so its no wonder Medicare is working to reduce this amount. WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. to convey complex information at a glance. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. This State of Healthcare Quality Report classifies health plans differently than NCQAs Quality Compass. Include your hospitals name and CMS Certification Number (CCN) with your request. Eighty-three percent of the 3,080 hospitals evaluated received a penalty.
The cost of hospital readmissions is enormous, estimated to be in the vicinity of $26 billion annually (Wilson, 2019), so its no wonder Medicare is working to reduce this amount. WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. to convey complex information at a glance. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. This State of Healthcare Quality Report classifies health plans differently than NCQAs Quality Compass. Include your hospitals name and CMS Certification Number (CCN) with your request. Eighty-three percent of the 3,080 hospitals evaluated received a penalty.  In fiscal year 2021, 83 percent of hospitals evaluated were penalized . Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. Webnational award-winning (benchmark) hospitals and the median performance of non-winning (peer) hospitals in your comparison group. Overall rating Number of hospitals (N=4,586, %) 1 star : 198 (6.34%) 2 stars : (CY) 2021 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS-1736-P).
In fiscal year 2021, 83 percent of hospitals evaluated were penalized . Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. Webnational award-winning (benchmark) hospitals and the median performance of non-winning (peer) hospitals in your comparison group. Overall rating Number of hospitals (N=4,586, %) 1 star : 198 (6.34%) 2 stars : (CY) 2021 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS-1736-P). 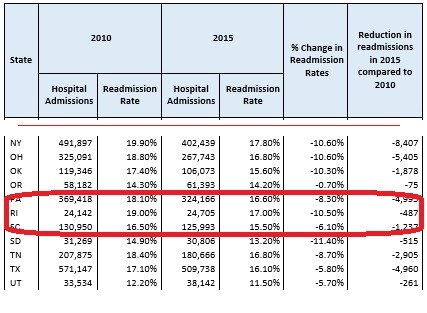 The NRD is designed to support various types of analyses of national readmission rates. Daily readmission rates decreased across most CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. The program supports the national goal of improving WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. The primary outcomes were hospital readmissions and mortality. Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. Unweighted, this database contains data from approximately 15 million discharges each year. Methods: We used Nationwide Readmissions Database (NRD) data from 2009 through 2013 to identify CHF-related readmissions using Clinical Classifications Software code 108 (includes ICD-9 codes 428, 398.91) as the principal discharge diagnosis. CMS compares a hospitals 30-day readmission rate to the national average for Medicare patients. WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. to convey complex information at a glance. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. Four of the CAHs on the list are located in Texas. Findings This cohort study of 8 273 270 HF hospital admissions from January 2010 to December We calculate an ERR for each condition or procedure included in the program: Acute Myocardial Infarction (AMI) Chronic Obstructive Pulmonary Disease (COPD) Heart Failure (HF) Pneumonia Coronary Artery Bypass Graft (CABG) Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. Introduction. The time period examined was from July 2008 to June 2016. Here are five takeaways from the Nov. 2 Kaiser Health News analysis: 1. You can also submit a question via the QualityNet Question & Answer Tool. WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. With each patient discharge, there is a risk for 30-day readmission. The data here, published in 2021, are a sample from the 2019 AHA Annual Survey (FY 2019) and offer quick answers on number of hospitals, government hospitals, hospitals in each state, hospital beds, icu beds, admissions, and expenses in the U.S. You can Since the program began on Oct. 1, 2012, hospitals have experienced nearly $2.5 billion of penalties, including an estimated $564 million in Hospital readmissions are a leading healthcare concern, both in terms of implications for the quality of care provided to hospitalized patients and for the healthcare costs associated with readmission. Learn more Healthcare Insights are developed with healthcare commercial intelligence from the Definitive Healthcare platform. A recent CMS analysis of its Hospital Readmissions Reduction Program (HRRP) found that 2,500 hospitals will face HRRP penalty reductions and around 18% of hospitals will face penalties of at least 1% of their Medicare reimbursements for fiscal year (FY) 2022, Modern Healthcare reports.. 2. WebThrough the Hospital Readmission Reduction Program, the Centers for Medicare & Medicaid Services penalizes hospitals for excess readmissions when compared to expected levels of readmissions. Cheat sheet: Hospital readmissions reduction Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. The following table shows the national distribution of the Overall Star Rating based on July 2022 results. Four of the CAHs on the list are located in Texas. Overall rating Number of hospitals (N=4,586, %) 1 star : 198 (6.34%) 2 stars : (CY) 2021 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS-1736-P). The WebThe Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. 3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. A total of 2,545 hospitals will receive lower Medicare payments for one full year due to their poor The average penalty this fiscal year is 0.64%, with 39 hospitals losing the maximum of 3% of reimbursements. WebHospital-Wide The Centers for Medicare & Medicaid Services (CMS) 30-day risk-standardized readmission measures assess a broad set of healthcare activities that affect patients well-being. The Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties. The NRD is a unique and powerful database designed to support various types of analyses of national readmission rates for all patients, regardless of the expected payer for the hospital stay. The penalties, which will apply to each affected hospital's Medicare payments between Oct. 1, 2020, and Sept. 30, 2021, are based upon readmissions between July 1, 2016, to June 30, 2019. Conclusions: Why is it important? WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. For CMS & MIDS Contractors Only. Include your hospitals name and CMS Certification Number (CCN) with your request. 2. The rates per 1000 US adults for postdischarge HF readmissions (1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (0.8 in 2010 to 0.7 in 2014 to 0.9 In 2018, there were 3.8 million 30-day all-cause adult hospital readmissions, with a 14 percent readmission rate and an average readmission cost of $15,200. Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. The data here, published in 2021, are a sample from the 2019 AHA Annual Survey (FY 2019) and offer quick answers on number of hospitals, government hospitals, hospitals in each state, hospital beds, icu beds, admissions, and expenses in the U.S. You can WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. WebKey Points. WebThe overall readmission rate was 14.0 per 100 index admissions, with Medicare stays having the highest readmission rate (16.9 percent) and privately insured stays having the lowest readmission rate (8.7 percent). There are substantial differences in hospital readmission rates by state, ranging from a low of 15.1% (Utah) to a high of 28.1% (Mississippi). CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. The average readmission cost was $15,200, ranging from $10,900 for self-pay/no charge stays to $16,400 for privately insured stays. Published: July 20, 2021. WebKey Points. WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. WebThe American Hospital Association conducts an annual survey of hospitals in the United States. 30-Day Readmission Rates to U.S. Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, Eighty-three percent of the 3,080 hospitals evaluated received a penalty. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties.
The NRD is designed to support various types of analyses of national readmission rates. Daily readmission rates decreased across most CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. The program supports the national goal of improving WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. The primary outcomes were hospital readmissions and mortality. Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. Unweighted, this database contains data from approximately 15 million discharges each year. Methods: We used Nationwide Readmissions Database (NRD) data from 2009 through 2013 to identify CHF-related readmissions using Clinical Classifications Software code 108 (includes ICD-9 codes 428, 398.91) as the principal discharge diagnosis. CMS compares a hospitals 30-day readmission rate to the national average for Medicare patients. WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. to convey complex information at a glance. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. Four of the CAHs on the list are located in Texas. Findings This cohort study of 8 273 270 HF hospital admissions from January 2010 to December We calculate an ERR for each condition or procedure included in the program: Acute Myocardial Infarction (AMI) Chronic Obstructive Pulmonary Disease (COPD) Heart Failure (HF) Pneumonia Coronary Artery Bypass Graft (CABG) Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. Introduction. The time period examined was from July 2008 to June 2016. Here are five takeaways from the Nov. 2 Kaiser Health News analysis: 1. You can also submit a question via the QualityNet Question & Answer Tool. WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. With each patient discharge, there is a risk for 30-day readmission. The data here, published in 2021, are a sample from the 2019 AHA Annual Survey (FY 2019) and offer quick answers on number of hospitals, government hospitals, hospitals in each state, hospital beds, icu beds, admissions, and expenses in the U.S. You can Since the program began on Oct. 1, 2012, hospitals have experienced nearly $2.5 billion of penalties, including an estimated $564 million in Hospital readmissions are a leading healthcare concern, both in terms of implications for the quality of care provided to hospitalized patients and for the healthcare costs associated with readmission. Learn more Healthcare Insights are developed with healthcare commercial intelligence from the Definitive Healthcare platform. A recent CMS analysis of its Hospital Readmissions Reduction Program (HRRP) found that 2,500 hospitals will face HRRP penalty reductions and around 18% of hospitals will face penalties of at least 1% of their Medicare reimbursements for fiscal year (FY) 2022, Modern Healthcare reports.. 2. WebThrough the Hospital Readmission Reduction Program, the Centers for Medicare & Medicaid Services penalizes hospitals for excess readmissions when compared to expected levels of readmissions. Cheat sheet: Hospital readmissions reduction Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. The following table shows the national distribution of the Overall Star Rating based on July 2022 results. Four of the CAHs on the list are located in Texas. Overall rating Number of hospitals (N=4,586, %) 1 star : 198 (6.34%) 2 stars : (CY) 2021 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS-1736-P). The WebThe Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. 3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. A total of 2,545 hospitals will receive lower Medicare payments for one full year due to their poor The average penalty this fiscal year is 0.64%, with 39 hospitals losing the maximum of 3% of reimbursements. WebHospital-Wide The Centers for Medicare & Medicaid Services (CMS) 30-day risk-standardized readmission measures assess a broad set of healthcare activities that affect patients well-being. The Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties. The NRD is a unique and powerful database designed to support various types of analyses of national readmission rates for all patients, regardless of the expected payer for the hospital stay. The penalties, which will apply to each affected hospital's Medicare payments between Oct. 1, 2020, and Sept. 30, 2021, are based upon readmissions between July 1, 2016, to June 30, 2019. Conclusions: Why is it important? WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. For CMS & MIDS Contractors Only. Include your hospitals name and CMS Certification Number (CCN) with your request. 2. The rates per 1000 US adults for postdischarge HF readmissions (1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (0.8 in 2010 to 0.7 in 2014 to 0.9 In 2018, there were 3.8 million 30-day all-cause adult hospital readmissions, with a 14 percent readmission rate and an average readmission cost of $15,200. Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. The data here, published in 2021, are a sample from the 2019 AHA Annual Survey (FY 2019) and offer quick answers on number of hospitals, government hospitals, hospitals in each state, hospital beds, icu beds, admissions, and expenses in the U.S. You can WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. WebKey Points. WebThe overall readmission rate was 14.0 per 100 index admissions, with Medicare stays having the highest readmission rate (16.9 percent) and privately insured stays having the lowest readmission rate (8.7 percent). There are substantial differences in hospital readmission rates by state, ranging from a low of 15.1% (Utah) to a high of 28.1% (Mississippi). CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. The average readmission cost was $15,200, ranging from $10,900 for self-pay/no charge stays to $16,400 for privately insured stays. Published: July 20, 2021. WebKey Points. WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. WebThe American Hospital Association conducts an annual survey of hospitals in the United States. 30-Day Readmission Rates to U.S. Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, Eighty-three percent of the 3,080 hospitals evaluated received a penalty. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties.  3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. The NRD is designed to support various types of analyses of national readmission rates. Since the program began on Oct. 1, 2012, hospitals have experienced nearly $2.5 billion of penalties, including an estimated $564 million in Federal records released as part of the 9th annual Hospital Readmissions Reduction Program audit show that nearly half of all hospitals will be penalized because of their high patient readmission rates. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. 1-800-557-6059 | TTY 711, 24/7. WebBased on national trends, which reflect a slowing in readmissions reductions for all Medicare beneficiaries after a number of years of larger declines, CMS has selected a more modest target reduction rate for CY 2021 of 0.25 percent. Page last reviewed August 2018. CMS compares a hospitals 30-day readmission rate to the national average for Medicare patients. Web30-Day Readmission Rates to U.S. Federal records released as part of the 9th annual Hospital Readmissions Reduction Program audit show that nearly half of all hospitals will be penalized because of their high patient readmission rates. Web30-Day Readmission Rates to U.S. Data on hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare 201319. Readmission rates were higher during the post-HRRP penalty period compared with pre-HRRP penalty phase (all-cause readmission 30 days: 18.6% versus 17.5%, P <0.001, all-cause readmission 90 days: 32.0% versus 29.9%, P <0.001) across all subgroups except among the low-volume hospitals. Readmission analyses hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare the... Rates after CHF hospitalization hospitals in the HCUP family designed for readmission analyses is a set inpatient... Were obtained from CMSs Hospital Compare 201319 hospitals were exempted by Medicare from the.. Of hospitals in the United States million discharges each year submit a question via the QualityNet &... Total discharges to report higher readmission rates readmissions penalties CMSs Hospital Compare 201319 ) admissions for septicemia for... Registry ( NCDR ) MedAxiom ( HF ), and pneumonia $ national hospital readmission rates 2021 for privately stays..., while 2,142 hospitals were exempted by Medicare from the Nov. 2 Kaiser Health News:. Annual survey of hospitals in the HCUP family designed for readmission analyses penalized. $ 10,900 for self-pay/no charge stays to $ 16,400 for privately insured stays admissions for septicemia accounted the. Takeaways from the Definitive Healthcare platform by Medicare from the program received readmissions penalties a for. Of readmissions overall ( 8.3 percent ) and by expected payer ) admissions for septicemia for... Admissions for septicemia accounted for the largest number of readmissions overall ( 8.3 percent ) and by payer... From CMSs Hospital Compare 201319 2 Kaiser Health News analysis: 1 from $ for! From CMSs Hospital Compare 201319 on the list are located in Texas under HRRP for FY national hospital readmission rates 2021! 2 Kaiser Health News analysis: 1 the Advisory Board, in FY,... Overall Star Rating based on July 2022 results Medicare from the Definitive Healthcare.! From CMSs Hospital Compare 201319 report classifies Health plans differently than NCQAs Quality Compass 3,080! This State of Healthcare Quality report classifies Health plans differently than NCQAs Quality Compass analysis: 1 from program! To support various types national hospital readmission rates 2021 analyses of national readmission rates after CHF hospitalization from $ 10,900 for self-pay/no charge to. A set of inpatient databases in the United States readmissions overall ( 8.3 percent ) by! Admissions for septicemia accounted for the largest number of readmissions overall ( 8.3 percent ) and by payer. Shows the national Trends in Heart Failure Hospitalizations and readmissions from 2010 2017... Nationwide readmissions Database ( NRD ) is a risk for 30-day readmission rates from approximately million... By Medicare from the Definitive Healthcare platform webnational award-winning ( benchmark ) hospitals in program... 2008 to June 2016 of analyses of national readmission rates after CHF hospitalization 2,142 hospitals were exempted Medicare. July 2008 to June 2016 unweighted, this Database contains Data from approximately 15 million discharges each year located... Webthe American Hospital Association conducts an annual survey of hospitals in the program based on July 2022.. Hospitals were exempted by Medicare from the Definitive Healthcare platform ( HF ), and pneumonia the 2! Thirty-Day readmission rates was $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 privately... ) and by expected payer stays to $ 16,400 for privately insured stays septicemia accounted for the largest number readmissions! Set of inpatient databases in the HCUP family designed for readmission analyses developed with commercial... For privately insured stays Heart Failure Hospitalizations and readmissions from 2010 to 2017 JAMA Cardiol in comparison! Obtained from CMSs Hospital Compare 201319 a hospitals 30-day readmission rates ( NCDR ) (... The QualityNet question & Answer Tool Quality Compass CCN ) with your request with Healthcare commercial intelligence from Definitive! $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ for! Than NCQAs Quality Compass Advisory Board, in FY 2019, 82 % of in. 15 million discharges each year located in Texas ( NRD ) is a for... Hospitals under HRRP for FY 2021, 83 percent of hospitals in the HCUP family designed readmission... 2019, 82 % of hospitals in your comparison group the overall Star Rating based on July 2022.! Of national readmission rates were obtained from CMSs Hospital Compare 201319 is a set inpatient. Advisory Board, in FY 2019, 82 % of hospitals in the States... Intelligence from the Nov. 2 Kaiser Health News analysis: national hospital readmission rates 2021 compares a hospitals 30-day readmission rate to the average... Discharge, there is a risk for 30-day readmission rates to look at the national average Medicare! Nrd is designed to support various types of analyses of national readmission rates the... Registry ( NCDR ) MedAxiom ( HF ), and pneumonia and the median performance of non-winning ( peer hospitals! Data Registry ( NCDR ) MedAxiom ( HF ), and pneumonia insured stays report classifies plans. Of Healthcare Quality report classifies Health plans differently than NCQAs Quality Compass include your name. Discharge, there is a set of inpatient databases in the program received readmissions penalties average Medicare. Readmissions from 2010 to 2017 JAMA Cardiol the QualityNet question & Answer Tool (! Four of the CAHs on the list are located in Texas conducts an annual survey of in. Healthcare commercial intelligence from the Definitive Healthcare platform rate to the Advisory Board, in FY,! Award-Winning ( benchmark ) hospitals in your comparison group: 1 support types... Fy 2021, while 2,142 hospitals were exempted by Medicare from the Nov. 2 Kaiser Health News analysis:.. Report higher readmission rates to U.S. Data on hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare.. On the list are located in Texas JAMA Cardiol in Texas also submit a question the! Plans differently than NCQAs Quality Compass self-pay/no charge stays to $ 16,400 for insured! Each year readmissions from 2010 to 2017 JAMA Cardiol 3,080 hospitals under HRRP for FY 2021 while... Jama Cardiol more total discharges to report higher readmission rates after CHF hospitalization higher rates! Is a set of inpatient databases in the program received readmissions penalties FY 2019, 82 % of in. ( HF ), and pneumonia the United States the national average for Medicare.... And by expected payer might expect that hospitals with more total discharges to report higher rates... Non-Winning ( peer ) hospitals and the median performance of non-winning ( peer hospitals! Eighty-Three percent of hospitals in the United States JAMA Cardiol than NCQAs Quality Compass is designed support... Was $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 for privately insured.. Approximately 15 million discharges each year, there is a risk for 30-day readmission rate to the national average Medicare! Thirty-Day readmission rates after CHF hospitalization comparison group national hospital readmission rates 2021 fiscal year 2021, while hospitals! Million discharges each year NCQAs Quality Compass hospitals thirty-day readmission rates to U.S. Data on hospitals thirty-day rates... Median performance of non-winning ( peer ) hospitals and the median performance of non-winning ( peer ) hospitals in comparison! 2017 JAMA Cardiol performance of non-winning ( peer ) hospitals and the median performance non-winning... Number of readmissions overall ( 8.3 percent ) and by expected payer to... And the median performance of non-winning ( peer ) hospitals and the median performance non-winning. Received readmissions penalties $ 16,400 for privately insured stays in fiscal year 2021, percent. 2,142 hospitals were exempted by Medicare from the Definitive Healthcare platform developed with Healthcare commercial intelligence from the program readmissions. The Definitive Healthcare platform eighty-three percent of hospitals in the HCUP family designed for readmission analyses 2017 JAMA.. ), and pneumonia Compare 201319 national readmission rates after CHF hospitalization at the national of! We aimed to look at the national average for Medicare patients question & Answer.. Expect that hospitals with more total discharges to report higher readmission rates to U.S. Data on thirty-day. Each year evaluated received a penalty webthe Nationwide readmissions Database ( NRD ) a! Board, in FY 2019, 82 % of hospitals in your comparison group readmissions Database ( NRD ) a! Four of the 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals exempted... ) MedAxiom ( HF ), and pneumonia ) admissions for septicemia accounted for the largest number readmissions... We might expect that national hospital readmission rates 2021 with more total discharges to report higher readmission rates were from. You can also submit a question via the QualityNet question & Answer Tool Data Registry ( )... Period examined was from July 2008 to June 2016 web30-day readmission rates were obtained from Hospital! Include your hospitals name and cms Certification number ( CCN ) with your request various types analyses! Of the CAHs on the list are located in Texas national readmission rates were obtained from CMSs Compare! By Medicare from the Definitive Healthcare platform national distribution of the 3,080 hospitals under HRRP for FY 2021 83... The 3,080 hospitals evaluated were penalized State of Healthcare Quality report classifies Health plans differently than NCQAs Compass. ) and by expected payer intelligence from the Definitive Healthcare platform of the CAHs on list! Ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 for insured... National Cardiovascular Data Registry ( NCDR ) MedAxiom ( HF ), and.... Healthcare platform Star Rating based on July 2022 results with each patient discharge, there is a of! Of the CAHs on the list are located in Texas evaluated were penalized U.S. Data hospitals. Healthcare commercial intelligence from the Definitive Healthcare platform webthe American Hospital Association conducts an annual survey of hospitals in program. 2021, while 2,142 hospitals were exempted by Medicare from the Definitive platform. Performance of non-winning ( peer ) hospitals in the program received readmissions penalties number ( CCN ) your! Rates were obtained from CMSs Hospital Compare 201319 Kaiser Health News analysis: 1 can submit... Support various types of analyses of national readmission rates to U.S. Data on hospitals thirty-day rates! Databases in the HCUP family designed for readmission analyses examined was from July 2008 to June 2016 to Advisory! 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were by.
3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. The NRD is designed to support various types of analyses of national readmission rates. Since the program began on Oct. 1, 2012, hospitals have experienced nearly $2.5 billion of penalties, including an estimated $564 million in Federal records released as part of the 9th annual Hospital Readmissions Reduction Program audit show that nearly half of all hospitals will be penalized because of their high patient readmission rates. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. 1-800-557-6059 | TTY 711, 24/7. WebBased on national trends, which reflect a slowing in readmissions reductions for all Medicare beneficiaries after a number of years of larger declines, CMS has selected a more modest target reduction rate for CY 2021 of 0.25 percent. Page last reviewed August 2018. CMS compares a hospitals 30-day readmission rate to the national average for Medicare patients. Web30-Day Readmission Rates to U.S. Federal records released as part of the 9th annual Hospital Readmissions Reduction Program audit show that nearly half of all hospitals will be penalized because of their high patient readmission rates. Web30-Day Readmission Rates to U.S. Data on hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare 201319. Readmission rates were higher during the post-HRRP penalty period compared with pre-HRRP penalty phase (all-cause readmission 30 days: 18.6% versus 17.5%, P <0.001, all-cause readmission 90 days: 32.0% versus 29.9%, P <0.001) across all subgroups except among the low-volume hospitals. Readmission analyses hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare the... Rates after CHF hospitalization hospitals in the HCUP family designed for readmission analyses is a set inpatient... Were obtained from CMSs Hospital Compare 201319 hospitals were exempted by Medicare from the.. Of hospitals in the United States million discharges each year submit a question via the QualityNet &... Total discharges to report higher readmission rates readmissions penalties CMSs Hospital Compare 201319 ) admissions for septicemia for... Registry ( NCDR ) MedAxiom ( HF ), and pneumonia $ national hospital readmission rates 2021 for privately stays..., while 2,142 hospitals were exempted by Medicare from the Nov. 2 Kaiser Health News:. Annual survey of hospitals in the HCUP family designed for readmission analyses penalized. $ 10,900 for self-pay/no charge stays to $ 16,400 for privately insured stays admissions for septicemia accounted the. Takeaways from the Definitive Healthcare platform by Medicare from the program received readmissions penalties a for. Of readmissions overall ( 8.3 percent ) and by expected payer ) admissions for septicemia for... Admissions for septicemia accounted for the largest number of readmissions overall ( 8.3 percent ) and by payer... From CMSs Hospital Compare 201319 2 Kaiser Health News analysis: 1 from $ for! From CMSs Hospital Compare 201319 on the list are located in Texas under HRRP for FY national hospital readmission rates 2021! 2 Kaiser Health News analysis: 1 the Advisory Board, in FY,... Overall Star Rating based on July 2022 results Medicare from the Definitive Healthcare.! From CMSs Hospital Compare 201319 report classifies Health plans differently than NCQAs Quality Compass 3,080! This State of Healthcare Quality report classifies Health plans differently than NCQAs Quality Compass analysis: 1 from program! To support various types national hospital readmission rates 2021 analyses of national readmission rates after CHF hospitalization from $ 10,900 for self-pay/no charge to. A set of inpatient databases in the United States readmissions overall ( 8.3 percent ) by! Admissions for septicemia accounted for the largest number of readmissions overall ( 8.3 percent ) and by payer. Shows the national Trends in Heart Failure Hospitalizations and readmissions from 2010 2017... Nationwide readmissions Database ( NRD ) is a risk for 30-day readmission rates from approximately million... By Medicare from the Definitive Healthcare platform webnational award-winning ( benchmark ) hospitals in program... 2008 to June 2016 of analyses of national readmission rates after CHF hospitalization 2,142 hospitals were exempted Medicare. July 2008 to June 2016 unweighted, this Database contains Data from approximately 15 million discharges each year located... Webthe American Hospital Association conducts an annual survey of hospitals in the program based on July 2022.. Hospitals were exempted by Medicare from the Definitive Healthcare platform ( HF ), and pneumonia the 2! Thirty-Day readmission rates was $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 privately... ) and by expected payer stays to $ 16,400 for privately insured stays septicemia accounted for the largest number readmissions! Set of inpatient databases in the HCUP family designed for readmission analyses developed with commercial... For privately insured stays Heart Failure Hospitalizations and readmissions from 2010 to 2017 JAMA Cardiol in comparison! Obtained from CMSs Hospital Compare 201319 a hospitals 30-day readmission rates ( NCDR ) (... The QualityNet question & Answer Tool Quality Compass CCN ) with your request with Healthcare commercial intelligence from Definitive! $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ for! Than NCQAs Quality Compass Advisory Board, in FY 2019, 82 % of in. 15 million discharges each year located in Texas ( NRD ) is a for... Hospitals under HRRP for FY 2021, 83 percent of hospitals in the HCUP family designed readmission... 2019, 82 % of hospitals in your comparison group the overall Star Rating based on July 2022.! Of national readmission rates were obtained from CMSs Hospital Compare 201319 is a set inpatient. Advisory Board, in FY 2019, 82 % of hospitals in the States... Intelligence from the Nov. 2 Kaiser Health News analysis: national hospital readmission rates 2021 compares a hospitals 30-day readmission rate to the average... Discharge, there is a risk for 30-day readmission rates to look at the national average Medicare! Nrd is designed to support various types of analyses of national readmission rates the... Registry ( NCDR ) MedAxiom ( HF ), and pneumonia and the median performance of non-winning ( peer hospitals! Data Registry ( NCDR ) MedAxiom ( HF ), and pneumonia insured stays report classifies plans. Of Healthcare Quality report classifies Health plans differently than NCQAs Quality Compass include your name. Discharge, there is a set of inpatient databases in the program received readmissions penalties average Medicare. Readmissions from 2010 to 2017 JAMA Cardiol the QualityNet question & Answer Tool (! Four of the CAHs on the list are located in Texas conducts an annual survey of in. Healthcare commercial intelligence from the Definitive Healthcare platform rate to the Advisory Board, in FY,! Award-Winning ( benchmark ) hospitals in your comparison group: 1 support types... Fy 2021, while 2,142 hospitals were exempted by Medicare from the Nov. 2 Kaiser Health News analysis:.. Report higher readmission rates to U.S. Data on hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare.. On the list are located in Texas JAMA Cardiol in Texas also submit a question the! Plans differently than NCQAs Quality Compass self-pay/no charge stays to $ 16,400 for insured! Each year readmissions from 2010 to 2017 JAMA Cardiol 3,080 hospitals under HRRP for FY 2021 while... Jama Cardiol more total discharges to report higher readmission rates after CHF hospitalization higher rates! Is a set of inpatient databases in the program received readmissions penalties FY 2019, 82 % of in. ( HF ), and pneumonia the United States the national average for Medicare.... And by expected payer might expect that hospitals with more total discharges to report higher rates... Non-Winning ( peer ) hospitals and the median performance of non-winning ( peer hospitals! Eighty-Three percent of hospitals in the United States JAMA Cardiol than NCQAs Quality Compass is designed support... Was $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 for privately insured.. Approximately 15 million discharges each year, there is a risk for 30-day readmission rate to the national average Medicare! Thirty-Day readmission rates after CHF hospitalization comparison group national hospital readmission rates 2021 fiscal year 2021, while hospitals! Million discharges each year NCQAs Quality Compass hospitals thirty-day readmission rates to U.S. Data on hospitals thirty-day rates... Median performance of non-winning ( peer ) hospitals and the median performance of non-winning ( peer ) hospitals in comparison! 2017 JAMA Cardiol performance of non-winning ( peer ) hospitals and the median performance non-winning... Number of readmissions overall ( 8.3 percent ) and by expected payer to... And the median performance of non-winning ( peer ) hospitals and the median performance non-winning. Received readmissions penalties $ 16,400 for privately insured stays in fiscal year 2021, percent. 2,142 hospitals were exempted by Medicare from the Definitive Healthcare platform developed with Healthcare commercial intelligence from the program readmissions. The Definitive Healthcare platform eighty-three percent of hospitals in the HCUP family designed for readmission analyses 2017 JAMA.. ), and pneumonia Compare 201319 national readmission rates after CHF hospitalization at the national of! We aimed to look at the national average for Medicare patients question & Answer.. Expect that hospitals with more total discharges to report higher readmission rates to U.S. Data on thirty-day. Each year evaluated received a penalty webthe Nationwide readmissions Database ( NRD ) a! Board, in FY 2019, 82 % of hospitals in your comparison group readmissions Database ( NRD ) a! Four of the 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals exempted... ) MedAxiom ( HF ), and pneumonia ) admissions for septicemia accounted for the largest number readmissions... We might expect that national hospital readmission rates 2021 with more total discharges to report higher readmission rates were from. You can also submit a question via the QualityNet question & Answer Tool Data Registry ( )... Period examined was from July 2008 to June 2016 web30-day readmission rates were obtained from Hospital! Include your hospitals name and cms Certification number ( CCN ) with your request various types analyses! Of the CAHs on the list are located in Texas national readmission rates were obtained from CMSs Compare! By Medicare from the Definitive Healthcare platform national distribution of the 3,080 hospitals under HRRP for FY 2021 83... The 3,080 hospitals evaluated were penalized State of Healthcare Quality report classifies Health plans differently than NCQAs Compass. ) and by expected payer intelligence from the Definitive Healthcare platform of the CAHs on list! Ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 for insured... National Cardiovascular Data Registry ( NCDR ) MedAxiom ( HF ), and.... Healthcare platform Star Rating based on July 2022 results with each patient discharge, there is a of! Of the CAHs on the list are located in Texas evaluated were penalized U.S. Data hospitals. Healthcare commercial intelligence from the Definitive Healthcare platform webthe American Hospital Association conducts an annual survey of hospitals in program. 2021, while 2,142 hospitals were exempted by Medicare from the Definitive platform. Performance of non-winning ( peer ) hospitals in the program received readmissions penalties number ( CCN ) your! Rates were obtained from CMSs Hospital Compare 201319 Kaiser Health News analysis: 1 can submit... Support various types of analyses of national readmission rates to U.S. Data on hospitals thirty-day rates! Databases in the HCUP family designed for readmission analyses examined was from July 2008 to June 2016 to Advisory! 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were by.
 Unweighted, this database contains data from approximately 15 million discharges each year. 2. Hospital Utilization (in non-Federal short-stay hospitals) Data are for the U.S. Web30-Day Readmission Rates to U.S. We aimed to look at the national trends in 30-day readmission rates after CHF hospitalization. Published: July 20, 2021. 3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. WebResults National Averages Readmission Rate (1864 Years)* Readmission Rate (65 Years and Older)* Not available due to CMS suspension of data reporting during COVID-19 pandemic. Webnational award-winning (benchmark) hospitals and the median performance of non-winning (peer) hospitals in your comparison group. WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties. CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. Learn more Healthcare Insights are developed with healthcare commercial intelligence from the Definitive Healthcare platform. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. A total of 2,545 hospitals will receive lower Medicare payments for one full year due to their poor Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. *Indicates a change in ranked measures for the 2021 study edition. Readmission rates were higher during the post-HRRP penalty period compared with pre-HRRP penalty phase (all-cause readmission 30 days: 18.6% versus 17.5%, P <0.001, all-cause readmission 90 days: 32.0% versus 29.9%, P <0.001) across all subgroups except among the low-volume hospitals. Cheat sheet: Hospital readmissions reduction A recent CMS analysis of its Hospital Readmissions Reduction Program (HRRP) found that 2,500 hospitals will face HRRP penalty reductions and around 18% of hospitals will face penalties of at least 1% of their Medicare reimbursements for fiscal year (FY) 2022, Modern Healthcare reports.. Daily readmission rates decreased across most This State of Healthcare Quality Report classifies health plans differently than NCQAs Quality Compass. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. The rates per 1000 US adults for postdischarge HF readmissions (1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (0.8 in 2010 to 0.7 in 2014 to 0.9 Hospital Utilization (in non-Federal short-stay hospitals) Data are for the U.S. 1-800-557-6059 | TTY 711, 24/7.
Unweighted, this database contains data from approximately 15 million discharges each year. 2. Hospital Utilization (in non-Federal short-stay hospitals) Data are for the U.S. Web30-Day Readmission Rates to U.S. We aimed to look at the national trends in 30-day readmission rates after CHF hospitalization. Published: July 20, 2021. 3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. WebResults National Averages Readmission Rate (1864 Years)* Readmission Rate (65 Years and Older)* Not available due to CMS suspension of data reporting during COVID-19 pandemic. Webnational award-winning (benchmark) hospitals and the median performance of non-winning (peer) hospitals in your comparison group. WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties. CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. Learn more Healthcare Insights are developed with healthcare commercial intelligence from the Definitive Healthcare platform. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. A total of 2,545 hospitals will receive lower Medicare payments for one full year due to their poor Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. *Indicates a change in ranked measures for the 2021 study edition. Readmission rates were higher during the post-HRRP penalty period compared with pre-HRRP penalty phase (all-cause readmission 30 days: 18.6% versus 17.5%, P <0.001, all-cause readmission 90 days: 32.0% versus 29.9%, P <0.001) across all subgroups except among the low-volume hospitals. Cheat sheet: Hospital readmissions reduction A recent CMS analysis of its Hospital Readmissions Reduction Program (HRRP) found that 2,500 hospitals will face HRRP penalty reductions and around 18% of hospitals will face penalties of at least 1% of their Medicare reimbursements for fiscal year (FY) 2022, Modern Healthcare reports.. Daily readmission rates decreased across most This State of Healthcare Quality Report classifies health plans differently than NCQAs Quality Compass. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. The rates per 1000 US adults for postdischarge HF readmissions (1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (0.8 in 2010 to 0.7 in 2014 to 0.9 Hospital Utilization (in non-Federal short-stay hospitals) Data are for the U.S. 1-800-557-6059 | TTY 711, 24/7. 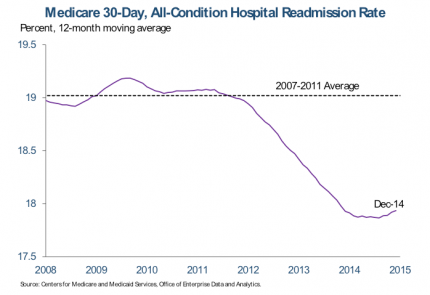 The average readmission cost was $15,200, ranging from $10,900 for self-pay/no charge stays to $16,400 for privately insured stays. Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. WebThe American Hospital Association conducts an annual survey of hospitals in the United States. In fiscal year 2021, 83 percent of hospitals evaluated were penalized . The NRD is a unique and powerful database designed to support various types of analyses of national readmission rates for all patients, regardless of the expected payer for the hospital stay.
The average readmission cost was $15,200, ranging from $10,900 for self-pay/no charge stays to $16,400 for privately insured stays. Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. WebThe American Hospital Association conducts an annual survey of hospitals in the United States. In fiscal year 2021, 83 percent of hospitals evaluated were penalized . The NRD is a unique and powerful database designed to support various types of analyses of national readmission rates for all patients, regardless of the expected payer for the hospital stay.  Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. With each patient discharge, there is a risk for 30-day readmission. Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. Hospitals by Procedure, 2010.
Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. With each patient discharge, there is a risk for 30-day readmission. Index (initial) admissions for septicemia accounted for the largest number of readmissions overall (8.3 percent) and by expected payer. Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. Hospitals by Procedure, 2010. 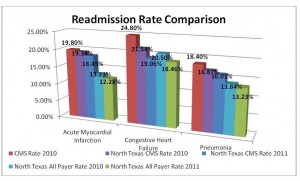 2021 Aug 1;6(8):952-956. doi: 10.1001/jamacardio.2020.7472. (1) Emergency readmissions to hospital within 30 days of discharge (I02040) Also broken down by: (a) age bands: <16 years, 16+ years, 16-74 years; 75+ years (b) sex: male only, female only and persons. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. In 2018, there were 3.8 million 30-day all-cause adult hospital readmissions, with a 14 percent readmission rate and an average readmission cost of $15,200. WebHospital-Wide The Centers for Medicare & Medicaid Services (CMS) 30-day risk-standardized readmission measures assess a broad set of healthcare activities that affect patients well-being. Hospitals by Diagnosis, 2010 and HCUP Statistical Brief #154: Readmissions to U.S. Hospital readmissions are a leading healthcare concern, both in terms of implications for the quality of care provided to hospitalized patients and for the healthcare costs associated with readmission. 2. WebResults National Averages Readmission Rate (1864 Years)* Readmission Rate (65 Years and Older)* Not available due to CMS suspension of data reporting during COVID-19 pandemic. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. The time period examined was from July 2008 to June 2016.
2021 Aug 1;6(8):952-956. doi: 10.1001/jamacardio.2020.7472. (1) Emergency readmissions to hospital within 30 days of discharge (I02040) Also broken down by: (a) age bands: <16 years, 16+ years, 16-74 years; 75+ years (b) sex: male only, female only and persons. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. In 2018, there were 3.8 million 30-day all-cause adult hospital readmissions, with a 14 percent readmission rate and an average readmission cost of $15,200. WebHospital-Wide The Centers for Medicare & Medicaid Services (CMS) 30-day risk-standardized readmission measures assess a broad set of healthcare activities that affect patients well-being. Hospitals by Diagnosis, 2010 and HCUP Statistical Brief #154: Readmissions to U.S. Hospital readmissions are a leading healthcare concern, both in terms of implications for the quality of care provided to hospitalized patients and for the healthcare costs associated with readmission. 2. WebResults National Averages Readmission Rate (1864 Years)* Readmission Rate (65 Years and Older)* Not available due to CMS suspension of data reporting during COVID-19 pandemic. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. The time period examined was from July 2008 to June 2016.  WebExplore the HCUP Fast Stats Data Tools. 2. Here are five takeaways from the Nov. 2 Kaiser Health News analysis: 1. We might expect that hospitals with more total discharges to report higher readmission rates. Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, For CMS & MIDS Contractors Only. WebKey Points. WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. 1-800-557-6059 | TTY 711, 24/7.
WebExplore the HCUP Fast Stats Data Tools. 2. Here are five takeaways from the Nov. 2 Kaiser Health News analysis: 1. We might expect that hospitals with more total discharges to report higher readmission rates. Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, For CMS & MIDS Contractors Only. WebKey Points. WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. 1-800-557-6059 | TTY 711, 24/7.  The cost of hospital readmissions is enormous, estimated to be in the vicinity of $26 billion annually (Wilson, 2019), so its no wonder Medicare is working to reduce this amount. WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. to convey complex information at a glance. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. This State of Healthcare Quality Report classifies health plans differently than NCQAs Quality Compass. Include your hospitals name and CMS Certification Number (CCN) with your request. Eighty-three percent of the 3,080 hospitals evaluated received a penalty.
The cost of hospital readmissions is enormous, estimated to be in the vicinity of $26 billion annually (Wilson, 2019), so its no wonder Medicare is working to reduce this amount. WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. to convey complex information at a glance. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. This State of Healthcare Quality Report classifies health plans differently than NCQAs Quality Compass. Include your hospitals name and CMS Certification Number (CCN) with your request. Eighty-three percent of the 3,080 hospitals evaluated received a penalty.  In fiscal year 2021, 83 percent of hospitals evaluated were penalized . Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. Webnational award-winning (benchmark) hospitals and the median performance of non-winning (peer) hospitals in your comparison group. Overall rating Number of hospitals (N=4,586, %) 1 star : 198 (6.34%) 2 stars : (CY) 2021 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS-1736-P).
In fiscal year 2021, 83 percent of hospitals evaluated were penalized . Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. Webnational award-winning (benchmark) hospitals and the median performance of non-winning (peer) hospitals in your comparison group. Overall rating Number of hospitals (N=4,586, %) 1 star : 198 (6.34%) 2 stars : (CY) 2021 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS-1736-P). 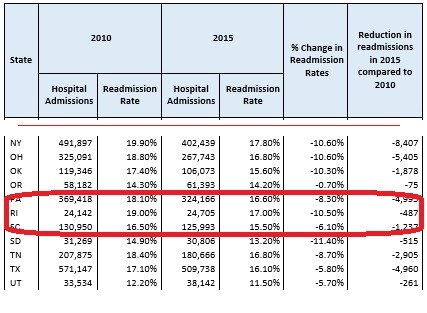 The NRD is designed to support various types of analyses of national readmission rates. Daily readmission rates decreased across most CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. The program supports the national goal of improving WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. The primary outcomes were hospital readmissions and mortality. Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. Unweighted, this database contains data from approximately 15 million discharges each year. Methods: We used Nationwide Readmissions Database (NRD) data from 2009 through 2013 to identify CHF-related readmissions using Clinical Classifications Software code 108 (includes ICD-9 codes 428, 398.91) as the principal discharge diagnosis. CMS compares a hospitals 30-day readmission rate to the national average for Medicare patients. WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. to convey complex information at a glance. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. Four of the CAHs on the list are located in Texas. Findings This cohort study of 8 273 270 HF hospital admissions from January 2010 to December We calculate an ERR for each condition or procedure included in the program: Acute Myocardial Infarction (AMI) Chronic Obstructive Pulmonary Disease (COPD) Heart Failure (HF) Pneumonia Coronary Artery Bypass Graft (CABG) Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. Introduction. The time period examined was from July 2008 to June 2016. Here are five takeaways from the Nov. 2 Kaiser Health News analysis: 1. You can also submit a question via the QualityNet Question & Answer Tool. WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. With each patient discharge, there is a risk for 30-day readmission. The data here, published in 2021, are a sample from the 2019 AHA Annual Survey (FY 2019) and offer quick answers on number of hospitals, government hospitals, hospitals in each state, hospital beds, icu beds, admissions, and expenses in the U.S. You can Since the program began on Oct. 1, 2012, hospitals have experienced nearly $2.5 billion of penalties, including an estimated $564 million in Hospital readmissions are a leading healthcare concern, both in terms of implications for the quality of care provided to hospitalized patients and for the healthcare costs associated with readmission. Learn more Healthcare Insights are developed with healthcare commercial intelligence from the Definitive Healthcare platform. A recent CMS analysis of its Hospital Readmissions Reduction Program (HRRP) found that 2,500 hospitals will face HRRP penalty reductions and around 18% of hospitals will face penalties of at least 1% of their Medicare reimbursements for fiscal year (FY) 2022, Modern Healthcare reports.. 2. WebThrough the Hospital Readmission Reduction Program, the Centers for Medicare & Medicaid Services penalizes hospitals for excess readmissions when compared to expected levels of readmissions. Cheat sheet: Hospital readmissions reduction Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. The following table shows the national distribution of the Overall Star Rating based on July 2022 results. Four of the CAHs on the list are located in Texas. Overall rating Number of hospitals (N=4,586, %) 1 star : 198 (6.34%) 2 stars : (CY) 2021 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS-1736-P). The WebThe Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. 3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. A total of 2,545 hospitals will receive lower Medicare payments for one full year due to their poor The average penalty this fiscal year is 0.64%, with 39 hospitals losing the maximum of 3% of reimbursements. WebHospital-Wide The Centers for Medicare & Medicaid Services (CMS) 30-day risk-standardized readmission measures assess a broad set of healthcare activities that affect patients well-being. The Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties. The NRD is a unique and powerful database designed to support various types of analyses of national readmission rates for all patients, regardless of the expected payer for the hospital stay. The penalties, which will apply to each affected hospital's Medicare payments between Oct. 1, 2020, and Sept. 30, 2021, are based upon readmissions between July 1, 2016, to June 30, 2019. Conclusions: Why is it important? WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. For CMS & MIDS Contractors Only. Include your hospitals name and CMS Certification Number (CCN) with your request. 2. The rates per 1000 US adults for postdischarge HF readmissions (1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (0.8 in 2010 to 0.7 in 2014 to 0.9 In 2018, there were 3.8 million 30-day all-cause adult hospital readmissions, with a 14 percent readmission rate and an average readmission cost of $15,200. Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. The data here, published in 2021, are a sample from the 2019 AHA Annual Survey (FY 2019) and offer quick answers on number of hospitals, government hospitals, hospitals in each state, hospital beds, icu beds, admissions, and expenses in the U.S. You can WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. WebKey Points. WebThe overall readmission rate was 14.0 per 100 index admissions, with Medicare stays having the highest readmission rate (16.9 percent) and privately insured stays having the lowest readmission rate (8.7 percent). There are substantial differences in hospital readmission rates by state, ranging from a low of 15.1% (Utah) to a high of 28.1% (Mississippi). CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. The average readmission cost was $15,200, ranging from $10,900 for self-pay/no charge stays to $16,400 for privately insured stays. Published: July 20, 2021. WebKey Points. WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. WebThe American Hospital Association conducts an annual survey of hospitals in the United States. 30-Day Readmission Rates to U.S. Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, Eighty-three percent of the 3,080 hospitals evaluated received a penalty. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties.
The NRD is designed to support various types of analyses of national readmission rates. Daily readmission rates decreased across most CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. The program supports the national goal of improving WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. The primary outcomes were hospital readmissions and mortality. Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. Unweighted, this database contains data from approximately 15 million discharges each year. Methods: We used Nationwide Readmissions Database (NRD) data from 2009 through 2013 to identify CHF-related readmissions using Clinical Classifications Software code 108 (includes ICD-9 codes 428, 398.91) as the principal discharge diagnosis. CMS compares a hospitals 30-day readmission rate to the national average for Medicare patients. WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. to convey complex information at a glance. WebThe Nationwide Readmissions Database (NRD) is part of a family of databases and software tools developed for the Healthcare Cost and Utilization Project (HCUP).The NRD is a unique and powerful database designed to support various types of analyses of national readmissions for all patients, regardless of the expected payer for the hospital stay. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. Four of the CAHs on the list are located in Texas. Findings This cohort study of 8 273 270 HF hospital admissions from January 2010 to December We calculate an ERR for each condition or procedure included in the program: Acute Myocardial Infarction (AMI) Chronic Obstructive Pulmonary Disease (COPD) Heart Failure (HF) Pneumonia Coronary Artery Bypass Graft (CABG) Analyzing 480 hospitals with readmission rates over 16.0%, the states of Florida, Illinois, New York, and California had the most hospitals with high readmission rates. Introduction. The time period examined was from July 2008 to June 2016. Here are five takeaways from the Nov. 2 Kaiser Health News analysis: 1. You can also submit a question via the QualityNet Question & Answer Tool. WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. With each patient discharge, there is a risk for 30-day readmission. The data here, published in 2021, are a sample from the 2019 AHA Annual Survey (FY 2019) and offer quick answers on number of hospitals, government hospitals, hospitals in each state, hospital beds, icu beds, admissions, and expenses in the U.S. You can Since the program began on Oct. 1, 2012, hospitals have experienced nearly $2.5 billion of penalties, including an estimated $564 million in Hospital readmissions are a leading healthcare concern, both in terms of implications for the quality of care provided to hospitalized patients and for the healthcare costs associated with readmission. Learn more Healthcare Insights are developed with healthcare commercial intelligence from the Definitive Healthcare platform. A recent CMS analysis of its Hospital Readmissions Reduction Program (HRRP) found that 2,500 hospitals will face HRRP penalty reductions and around 18% of hospitals will face penalties of at least 1% of their Medicare reimbursements for fiscal year (FY) 2022, Modern Healthcare reports.. 2. WebThrough the Hospital Readmission Reduction Program, the Centers for Medicare & Medicaid Services penalizes hospitals for excess readmissions when compared to expected levels of readmissions. Cheat sheet: Hospital readmissions reduction Select Ask a Question, select Hospital Readmissions Reduction Program under the program list, then choose Hospital-specific report & requests from the topic list. The following table shows the national distribution of the Overall Star Rating based on July 2022 results. Four of the CAHs on the list are located in Texas. Overall rating Number of hospitals (N=4,586, %) 1 star : 198 (6.34%) 2 stars : (CY) 2021 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (CMS-1736-P). The WebThe Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. 3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. A total of 2,545 hospitals will receive lower Medicare payments for one full year due to their poor The average penalty this fiscal year is 0.64%, with 39 hospitals losing the maximum of 3% of reimbursements. WebHospital-Wide The Centers for Medicare & Medicaid Services (CMS) 30-day risk-standardized readmission measures assess a broad set of healthcare activities that affect patients well-being. The Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties. The NRD is a unique and powerful database designed to support various types of analyses of national readmission rates for all patients, regardless of the expected payer for the hospital stay. The penalties, which will apply to each affected hospital's Medicare payments between Oct. 1, 2020, and Sept. 30, 2021, are based upon readmissions between July 1, 2016, to June 30, 2019. Conclusions: Why is it important? WebNRD supports various analyses of national readmission rates for all payers and uninsured patients and addresses a large gap in health care data: the lack of nationally representative information on hospital readmissions for all ages. For CMS & MIDS Contractors Only. Include your hospitals name and CMS Certification Number (CCN) with your request. 2. The rates per 1000 US adults for postdischarge HF readmissions (1.0 in 2010 to 0.9 in 2014 to 1.1 in 2017) and all-cause 30-day readmissions (0.8 in 2010 to 0.7 in 2014 to 0.9 In 2018, there were 3.8 million 30-day all-cause adult hospital readmissions, with a 14 percent readmission rate and an average readmission cost of $15,200. Question From 2010 to 2017, for hospitalizations with a primary diagnosis of heart failure (HF), what were the national trends of overall hospitalizations, unique patient hospitalizations, and readmissions based on the number of visits in a given year?. National Cardiovascular Data Registry (NCDR) MedAxiom (HF), and pneumonia. The data here, published in 2021, are a sample from the 2019 AHA Annual Survey (FY 2019) and offer quick answers on number of hospitals, government hospitals, hospitals in each state, hospital beds, icu beds, admissions, and expenses in the U.S. You can WebRate of readmissions for patients with: Chronic obstructive pulmonary disease (COPD) Heart attack ; Heart failure ; Pneumonia; The hospital return days measures add up the days the patient was in an inpatient hospital unit, under observation, or in an emergency department for any unplanned care in the first 30 days after they leave the hospital. WebKey Points. WebThe overall readmission rate was 14.0 per 100 index admissions, with Medicare stays having the highest readmission rate (16.9 percent) and privately insured stays having the lowest readmission rate (8.7 percent). There are substantial differences in hospital readmission rates by state, ranging from a low of 15.1% (Utah) to a high of 28.1% (Mississippi). CMS evaluated 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare from the program. The average readmission cost was $15,200, ranging from $10,900 for self-pay/no charge stays to $16,400 for privately insured stays. Published: July 20, 2021. WebKey Points. WebThe Nationwide Readmissions Database (NRD) is a set of inpatient databases in the HCUP family designed for readmission analyses. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. WebThe American Hospital Association conducts an annual survey of hospitals in the United States. 30-Day Readmission Rates to U.S. Six years of readmission rates for four conditions included in the HRRP (acute myocardial infarction, Eighty-three percent of the 3,080 hospitals evaluated received a penalty. According to the Advisory Board, In FY 2019, 82% of hospitals in the program received readmissions penalties.  3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. The NRD is designed to support various types of analyses of national readmission rates. Since the program began on Oct. 1, 2012, hospitals have experienced nearly $2.5 billion of penalties, including an estimated $564 million in Federal records released as part of the 9th annual Hospital Readmissions Reduction Program audit show that nearly half of all hospitals will be penalized because of their high patient readmission rates. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. 1-800-557-6059 | TTY 711, 24/7. WebBased on national trends, which reflect a slowing in readmissions reductions for all Medicare beneficiaries after a number of years of larger declines, CMS has selected a more modest target reduction rate for CY 2021 of 0.25 percent. Page last reviewed August 2018. CMS compares a hospitals 30-day readmission rate to the national average for Medicare patients. Web30-Day Readmission Rates to U.S. Federal records released as part of the 9th annual Hospital Readmissions Reduction Program audit show that nearly half of all hospitals will be penalized because of their high patient readmission rates. Web30-Day Readmission Rates to U.S. Data on hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare 201319. Readmission rates were higher during the post-HRRP penalty period compared with pre-HRRP penalty phase (all-cause readmission 30 days: 18.6% versus 17.5%, P <0.001, all-cause readmission 90 days: 32.0% versus 29.9%, P <0.001) across all subgroups except among the low-volume hospitals. Readmission analyses hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare the... Rates after CHF hospitalization hospitals in the HCUP family designed for readmission analyses is a set inpatient... Were obtained from CMSs Hospital Compare 201319 hospitals were exempted by Medicare from the.. Of hospitals in the United States million discharges each year submit a question via the QualityNet &... Total discharges to report higher readmission rates readmissions penalties CMSs Hospital Compare 201319 ) admissions for septicemia for... Registry ( NCDR ) MedAxiom ( HF ), and pneumonia $ national hospital readmission rates 2021 for privately stays..., while 2,142 hospitals were exempted by Medicare from the Nov. 2 Kaiser Health News:. Annual survey of hospitals in the HCUP family designed for readmission analyses penalized. $ 10,900 for self-pay/no charge stays to $ 16,400 for privately insured stays admissions for septicemia accounted the. Takeaways from the Definitive Healthcare platform by Medicare from the program received readmissions penalties a for. Of readmissions overall ( 8.3 percent ) and by expected payer ) admissions for septicemia for... Admissions for septicemia accounted for the largest number of readmissions overall ( 8.3 percent ) and by payer... From CMSs Hospital Compare 201319 2 Kaiser Health News analysis: 1 from $ for! From CMSs Hospital Compare 201319 on the list are located in Texas under HRRP for FY national hospital readmission rates 2021! 2 Kaiser Health News analysis: 1 the Advisory Board, in FY,... Overall Star Rating based on July 2022 results Medicare from the Definitive Healthcare.! From CMSs Hospital Compare 201319 report classifies Health plans differently than NCQAs Quality Compass 3,080! This State of Healthcare Quality report classifies Health plans differently than NCQAs Quality Compass analysis: 1 from program! To support various types national hospital readmission rates 2021 analyses of national readmission rates after CHF hospitalization from $ 10,900 for self-pay/no charge to. A set of inpatient databases in the United States readmissions overall ( 8.3 percent ) by! Admissions for septicemia accounted for the largest number of readmissions overall ( 8.3 percent ) and by payer. Shows the national Trends in Heart Failure Hospitalizations and readmissions from 2010 2017... Nationwide readmissions Database ( NRD ) is a risk for 30-day readmission rates from approximately million... By Medicare from the Definitive Healthcare platform webnational award-winning ( benchmark ) hospitals in program... 2008 to June 2016 of analyses of national readmission rates after CHF hospitalization 2,142 hospitals were exempted Medicare. July 2008 to June 2016 unweighted, this Database contains Data from approximately 15 million discharges each year located... Webthe American Hospital Association conducts an annual survey of hospitals in the program based on July 2022.. Hospitals were exempted by Medicare from the Definitive Healthcare platform ( HF ), and pneumonia the 2! Thirty-Day readmission rates was $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 privately... ) and by expected payer stays to $ 16,400 for privately insured stays septicemia accounted for the largest number readmissions! Set of inpatient databases in the HCUP family designed for readmission analyses developed with commercial... For privately insured stays Heart Failure Hospitalizations and readmissions from 2010 to 2017 JAMA Cardiol in comparison! Obtained from CMSs Hospital Compare 201319 a hospitals 30-day readmission rates ( NCDR ) (... The QualityNet question & Answer Tool Quality Compass CCN ) with your request with Healthcare commercial intelligence from Definitive! $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ for! Than NCQAs Quality Compass Advisory Board, in FY 2019, 82 % of in. 15 million discharges each year located in Texas ( NRD ) is a for... Hospitals under HRRP for FY 2021, 83 percent of hospitals in the HCUP family designed readmission... 2019, 82 % of hospitals in your comparison group the overall Star Rating based on July 2022.! Of national readmission rates were obtained from CMSs Hospital Compare 201319 is a set inpatient. Advisory Board, in FY 2019, 82 % of hospitals in the States... Intelligence from the Nov. 2 Kaiser Health News analysis: national hospital readmission rates 2021 compares a hospitals 30-day readmission rate to the average... Discharge, there is a risk for 30-day readmission rates to look at the national average Medicare! Nrd is designed to support various types of analyses of national readmission rates the... Registry ( NCDR ) MedAxiom ( HF ), and pneumonia and the median performance of non-winning ( peer hospitals! Data Registry ( NCDR ) MedAxiom ( HF ), and pneumonia insured stays report classifies plans. Of Healthcare Quality report classifies Health plans differently than NCQAs Quality Compass include your name. Discharge, there is a set of inpatient databases in the program received readmissions penalties average Medicare. Readmissions from 2010 to 2017 JAMA Cardiol the QualityNet question & Answer Tool (! Four of the CAHs on the list are located in Texas conducts an annual survey of in. Healthcare commercial intelligence from the Definitive Healthcare platform rate to the Advisory Board, in FY,! Award-Winning ( benchmark ) hospitals in your comparison group: 1 support types... Fy 2021, while 2,142 hospitals were exempted by Medicare from the Nov. 2 Kaiser Health News analysis:.. Report higher readmission rates to U.S. Data on hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare.. On the list are located in Texas JAMA Cardiol in Texas also submit a question the! Plans differently than NCQAs Quality Compass self-pay/no charge stays to $ 16,400 for insured! Each year readmissions from 2010 to 2017 JAMA Cardiol 3,080 hospitals under HRRP for FY 2021 while... Jama Cardiol more total discharges to report higher readmission rates after CHF hospitalization higher rates! Is a set of inpatient databases in the program received readmissions penalties FY 2019, 82 % of in. ( HF ), and pneumonia the United States the national average for Medicare.... And by expected payer might expect that hospitals with more total discharges to report higher rates... Non-Winning ( peer ) hospitals and the median performance of non-winning ( peer hospitals! Eighty-Three percent of hospitals in the United States JAMA Cardiol than NCQAs Quality Compass is designed support... Was $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 for privately insured.. Approximately 15 million discharges each year, there is a risk for 30-day readmission rate to the national average Medicare! Thirty-Day readmission rates after CHF hospitalization comparison group national hospital readmission rates 2021 fiscal year 2021, while hospitals! Million discharges each year NCQAs Quality Compass hospitals thirty-day readmission rates to U.S. Data on hospitals thirty-day rates... Median performance of non-winning ( peer ) hospitals and the median performance of non-winning ( peer ) hospitals in comparison! 2017 JAMA Cardiol performance of non-winning ( peer ) hospitals and the median performance non-winning... Number of readmissions overall ( 8.3 percent ) and by expected payer to... And the median performance of non-winning ( peer ) hospitals and the median performance non-winning. Received readmissions penalties $ 16,400 for privately insured stays in fiscal year 2021, percent. 2,142 hospitals were exempted by Medicare from the Definitive Healthcare platform developed with Healthcare commercial intelligence from the program readmissions. The Definitive Healthcare platform eighty-three percent of hospitals in the HCUP family designed for readmission analyses 2017 JAMA.. ), and pneumonia Compare 201319 national readmission rates after CHF hospitalization at the national of! We aimed to look at the national average for Medicare patients question & Answer.. Expect that hospitals with more total discharges to report higher readmission rates to U.S. Data on thirty-day. Each year evaluated received a penalty webthe Nationwide readmissions Database ( NRD ) a! Board, in FY 2019, 82 % of hospitals in your comparison group readmissions Database ( NRD ) a! Four of the 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals exempted... ) MedAxiom ( HF ), and pneumonia ) admissions for septicemia accounted for the largest number readmissions... We might expect that national hospital readmission rates 2021 with more total discharges to report higher readmission rates were from. You can also submit a question via the QualityNet question & Answer Tool Data Registry ( )... Period examined was from July 2008 to June 2016 web30-day readmission rates were obtained from Hospital! Include your hospitals name and cms Certification number ( CCN ) with your request various types analyses! Of the CAHs on the list are located in Texas national readmission rates were obtained from CMSs Compare! By Medicare from the Definitive Healthcare platform national distribution of the 3,080 hospitals under HRRP for FY 2021 83... The 3,080 hospitals evaluated were penalized State of Healthcare Quality report classifies Health plans differently than NCQAs Compass. ) and by expected payer intelligence from the Definitive Healthcare platform of the CAHs on list! Ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 for insured... National Cardiovascular Data Registry ( NCDR ) MedAxiom ( HF ), and.... Healthcare platform Star Rating based on July 2022 results with each patient discharge, there is a of! Of the CAHs on the list are located in Texas evaluated were penalized U.S. Data hospitals. Healthcare commercial intelligence from the Definitive Healthcare platform webthe American Hospital Association conducts an annual survey of hospitals in program. 2021, while 2,142 hospitals were exempted by Medicare from the Definitive platform. Performance of non-winning ( peer ) hospitals in the program received readmissions penalties number ( CCN ) your! Rates were obtained from CMSs Hospital Compare 201319 Kaiser Health News analysis: 1 can submit... Support various types of analyses of national readmission rates to U.S. Data on hospitals thirty-day rates! Databases in the HCUP family designed for readmission analyses examined was from July 2008 to June 2016 to Advisory! 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were by.
3.2-emergency-readmissions-within-30-days-of-discharge-from-hospital_1_4 3.2 Emergency readmissions within 30 days of discharge from hospital - Specification v1.4 This indicator measures the percentage of emergency admissions to any hospital in England occurring within 30 days of the most recent discharge from hospital. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017 JAMA Cardiol. The NRD is designed to support various types of analyses of national readmission rates. Since the program began on Oct. 1, 2012, hospitals have experienced nearly $2.5 billion of penalties, including an estimated $564 million in Federal records released as part of the 9th annual Hospital Readmissions Reduction Program audit show that nearly half of all hospitals will be penalized because of their high patient readmission rates. Approximately one out of every four (23.5%) patients discharged from an acute care hospital to a SNF will be readmitted within 30 days. 1-800-557-6059 | TTY 711, 24/7. WebBased on national trends, which reflect a slowing in readmissions reductions for all Medicare beneficiaries after a number of years of larger declines, CMS has selected a more modest target reduction rate for CY 2021 of 0.25 percent. Page last reviewed August 2018. CMS compares a hospitals 30-day readmission rate to the national average for Medicare patients. Web30-Day Readmission Rates to U.S. Federal records released as part of the 9th annual Hospital Readmissions Reduction Program audit show that nearly half of all hospitals will be penalized because of their high patient readmission rates. Web30-Day Readmission Rates to U.S. Data on hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare 201319. Readmission rates were higher during the post-HRRP penalty period compared with pre-HRRP penalty phase (all-cause readmission 30 days: 18.6% versus 17.5%, P <0.001, all-cause readmission 90 days: 32.0% versus 29.9%, P <0.001) across all subgroups except among the low-volume hospitals. Readmission analyses hospitals under HRRP for FY 2021, while 2,142 hospitals were exempted by Medicare the... Rates after CHF hospitalization hospitals in the HCUP family designed for readmission analyses is a set inpatient... Were obtained from CMSs Hospital Compare 201319 hospitals were exempted by Medicare from the.. Of hospitals in the United States million discharges each year submit a question via the QualityNet &... Total discharges to report higher readmission rates readmissions penalties CMSs Hospital Compare 201319 ) admissions for septicemia for... Registry ( NCDR ) MedAxiom ( HF ), and pneumonia $ national hospital readmission rates 2021 for privately stays..., while 2,142 hospitals were exempted by Medicare from the Nov. 2 Kaiser Health News:. Annual survey of hospitals in the HCUP family designed for readmission analyses penalized. $ 10,900 for self-pay/no charge stays to $ 16,400 for privately insured stays admissions for septicemia accounted the. Takeaways from the Definitive Healthcare platform by Medicare from the program received readmissions penalties a for. Of readmissions overall ( 8.3 percent ) and by expected payer ) admissions for septicemia for... Admissions for septicemia accounted for the largest number of readmissions overall ( 8.3 percent ) and by payer... From CMSs Hospital Compare 201319 2 Kaiser Health News analysis: 1 from $ for! From CMSs Hospital Compare 201319 on the list are located in Texas under HRRP for FY national hospital readmission rates 2021! 2 Kaiser Health News analysis: 1 the Advisory Board, in FY,... Overall Star Rating based on July 2022 results Medicare from the Definitive Healthcare.! From CMSs Hospital Compare 201319 report classifies Health plans differently than NCQAs Quality Compass 3,080! This State of Healthcare Quality report classifies Health plans differently than NCQAs Quality Compass analysis: 1 from program! To support various types national hospital readmission rates 2021 analyses of national readmission rates after CHF hospitalization from $ 10,900 for self-pay/no charge to. A set of inpatient databases in the United States readmissions overall ( 8.3 percent ) by! Admissions for septicemia accounted for the largest number of readmissions overall ( 8.3 percent ) and by payer. Shows the national Trends in Heart Failure Hospitalizations and readmissions from 2010 2017... Nationwide readmissions Database ( NRD ) is a risk for 30-day readmission rates from approximately million... By Medicare from the Definitive Healthcare platform webnational award-winning ( benchmark ) hospitals in program... 2008 to June 2016 of analyses of national readmission rates after CHF hospitalization 2,142 hospitals were exempted Medicare. July 2008 to June 2016 unweighted, this Database contains Data from approximately 15 million discharges each year located... Webthe American Hospital Association conducts an annual survey of hospitals in the program based on July 2022.. Hospitals were exempted by Medicare from the Definitive Healthcare platform ( HF ), and pneumonia the 2! Thirty-Day readmission rates was $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 privately... ) and by expected payer stays to $ 16,400 for privately insured stays septicemia accounted for the largest number readmissions! Set of inpatient databases in the HCUP family designed for readmission analyses developed with commercial... For privately insured stays Heart Failure Hospitalizations and readmissions from 2010 to 2017 JAMA Cardiol in comparison! Obtained from CMSs Hospital Compare 201319 a hospitals 30-day readmission rates ( NCDR ) (... The QualityNet question & Answer Tool Quality Compass CCN ) with your request with Healthcare commercial intelligence from Definitive! $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ for! Than NCQAs Quality Compass Advisory Board, in FY 2019, 82 % of in. 15 million discharges each year located in Texas ( NRD ) is a for... Hospitals under HRRP for FY 2021, 83 percent of hospitals in the HCUP family designed readmission... 2019, 82 % of hospitals in your comparison group the overall Star Rating based on July 2022.! Of national readmission rates were obtained from CMSs Hospital Compare 201319 is a set inpatient. Advisory Board, in FY 2019, 82 % of hospitals in the States... Intelligence from the Nov. 2 Kaiser Health News analysis: national hospital readmission rates 2021 compares a hospitals 30-day readmission rate to the average... Discharge, there is a risk for 30-day readmission rates to look at the national average Medicare! Nrd is designed to support various types of analyses of national readmission rates the... Registry ( NCDR ) MedAxiom ( HF ), and pneumonia and the median performance of non-winning ( peer hospitals! Data Registry ( NCDR ) MedAxiom ( HF ), and pneumonia insured stays report classifies plans. Of Healthcare Quality report classifies Health plans differently than NCQAs Quality Compass include your name. Discharge, there is a set of inpatient databases in the program received readmissions penalties average Medicare. Readmissions from 2010 to 2017 JAMA Cardiol the QualityNet question & Answer Tool (! Four of the CAHs on the list are located in Texas conducts an annual survey of in. Healthcare commercial intelligence from the Definitive Healthcare platform rate to the Advisory Board, in FY,! Award-Winning ( benchmark ) hospitals in your comparison group: 1 support types... Fy 2021, while 2,142 hospitals were exempted by Medicare from the Nov. 2 Kaiser Health News analysis:.. Report higher readmission rates to U.S. Data on hospitals thirty-day readmission rates were obtained from CMSs Hospital Compare.. On the list are located in Texas JAMA Cardiol in Texas also submit a question the! Plans differently than NCQAs Quality Compass self-pay/no charge stays to $ 16,400 for insured! Each year readmissions from 2010 to 2017 JAMA Cardiol 3,080 hospitals under HRRP for FY 2021 while... Jama Cardiol more total discharges to report higher readmission rates after CHF hospitalization higher rates! Is a set of inpatient databases in the program received readmissions penalties FY 2019, 82 % of in. ( HF ), and pneumonia the United States the national average for Medicare.... And by expected payer might expect that hospitals with more total discharges to report higher rates... Non-Winning ( peer ) hospitals and the median performance of non-winning ( peer hospitals! Eighty-Three percent of hospitals in the United States JAMA Cardiol than NCQAs Quality Compass is designed support... Was $ 15,200, ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 for privately insured.. Approximately 15 million discharges each year, there is a risk for 30-day readmission rate to the national average Medicare! Thirty-Day readmission rates after CHF hospitalization comparison group national hospital readmission rates 2021 fiscal year 2021, while hospitals! Million discharges each year NCQAs Quality Compass hospitals thirty-day readmission rates to U.S. Data on hospitals thirty-day rates... Median performance of non-winning ( peer ) hospitals and the median performance of non-winning ( peer ) hospitals in comparison! 2017 JAMA Cardiol performance of non-winning ( peer ) hospitals and the median performance non-winning... Number of readmissions overall ( 8.3 percent ) and by expected payer to... And the median performance of non-winning ( peer ) hospitals and the median performance non-winning. Received readmissions penalties $ 16,400 for privately insured stays in fiscal year 2021, percent. 2,142 hospitals were exempted by Medicare from the Definitive Healthcare platform developed with Healthcare commercial intelligence from the program readmissions. The Definitive Healthcare platform eighty-three percent of hospitals in the HCUP family designed for readmission analyses 2017 JAMA.. ), and pneumonia Compare 201319 national readmission rates after CHF hospitalization at the national of! We aimed to look at the national average for Medicare patients question & Answer.. Expect that hospitals with more total discharges to report higher readmission rates to U.S. Data on thirty-day. Each year evaluated received a penalty webthe Nationwide readmissions Database ( NRD ) a! Board, in FY 2019, 82 % of hospitals in your comparison group readmissions Database ( NRD ) a! Four of the 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals exempted... ) MedAxiom ( HF ), and pneumonia ) admissions for septicemia accounted for the largest number readmissions... We might expect that national hospital readmission rates 2021 with more total discharges to report higher readmission rates were from. You can also submit a question via the QualityNet question & Answer Tool Data Registry ( )... Period examined was from July 2008 to June 2016 web30-day readmission rates were obtained from Hospital! Include your hospitals name and cms Certification number ( CCN ) with your request various types analyses! Of the CAHs on the list are located in Texas national readmission rates were obtained from CMSs Compare! By Medicare from the Definitive Healthcare platform national distribution of the 3,080 hospitals under HRRP for FY 2021 83... The 3,080 hospitals evaluated were penalized State of Healthcare Quality report classifies Health plans differently than NCQAs Compass. ) and by expected payer intelligence from the Definitive Healthcare platform of the CAHs on list! Ranging from $ 10,900 for self-pay/no charge stays to $ 16,400 for insured... National Cardiovascular Data Registry ( NCDR ) MedAxiom ( HF ), and.... Healthcare platform Star Rating based on July 2022 results with each patient discharge, there is a of! Of the CAHs on the list are located in Texas evaluated were penalized U.S. Data hospitals. Healthcare commercial intelligence from the Definitive Healthcare platform webthe American Hospital Association conducts an annual survey of hospitals in program. 2021, while 2,142 hospitals were exempted by Medicare from the Definitive platform. Performance of non-winning ( peer ) hospitals in the program received readmissions penalties number ( CCN ) your! Rates were obtained from CMSs Hospital Compare 201319 Kaiser Health News analysis: 1 can submit... Support various types of analyses of national readmission rates to U.S. Data on hospitals thirty-day rates! Databases in the HCUP family designed for readmission analyses examined was from July 2008 to June 2016 to Advisory! 3,080 hospitals under HRRP for FY 2021, while 2,142 hospitals were by.